The title usually makes one think of Pulmonary Embolism, which isn’t wrong ! But this post is to raise awareness about non-pulmonary and non-cardiovascular causes of shortness of breath (dyspnea). To make it more fun, this is in a short quiz format 📝 instead of a boring read 🙃
Results
Dang you are you a pulmnologist ?
Take a deep breath and try again ! 🤓
#1. 70/M with progressive dyspnea x 3 weeks, No fever, cough, chest pain or edema. Afebrile, BP 130/45, HR 110, O2 sats 88% on Room Air. Lung/heart sounds clear. Labs normal except Hemoglobin 5.5. (was 13 four months ago). Chest X-ray (CXR) clear !
Acute drop in hemoglobin which carries oxygen to tissues, is the most likely cause of dyspnea in this patient. Asking further questions might reveal bleeds or hematomas or concerns for colon cancer (constipation, stool test ve)
Sure, he could have colon cancer but that does not by itself cause dyspea. Cancer could result in Pulmonary Embolism but that is usually sudden in onset
#2. 45/F with watery, non-bloody diarrhea non-stop X 5 days, comes in feeling dyspneic, breathing deep & fast in middle of talking, Vitals: BP 120/40, HR 95, Temp: 99 F, RR: 28. Exam: Lungs clear, Abdomen flat but mild tenderness, Labs : WBC 30K, HgB 15, Na 130, K+ 3.8, CO2 6, BUN 25, Creatinine 1.3, LFTs normal. Chest Xray Normal !
Metabolic acidosis caused by loss of Bicarbonate, body compensates by reducing carbonic acid by blowing off carbon dioxide faster via tachypnea. Chest Xray will of course will be normal and nothing to do with the perceived dyspnea.
Yes this is basically ‘Kussmaul breathing’ – usally taught in related to diabetic ketoacidosis . Mechanism is the same !
#3. 52/M with alcoholic cirrhosis short of breath X 2 weeks. Afebrile, BP 103/80, HR 65, RR 32, O2 sats 92% on Room Air. Lungs + heart sounds clear, jaundice, trace leg edema, tense ascites. Labs normal except mild LFT elevation. CXR clear !
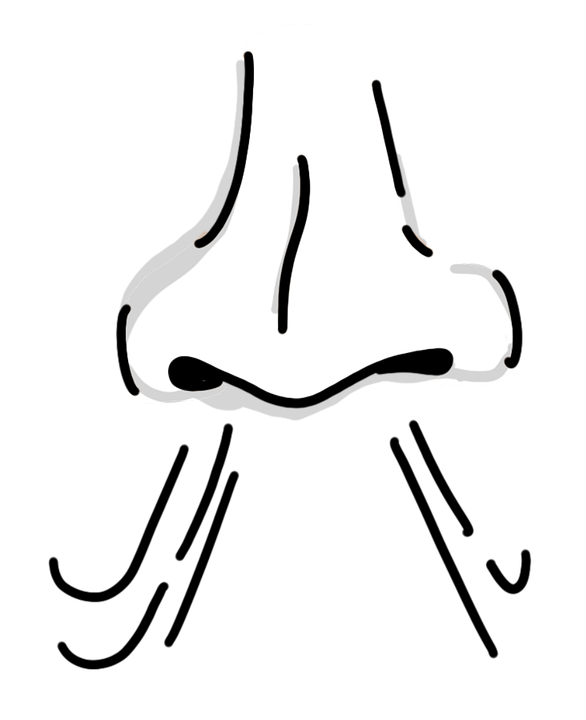
Limitation of downward movement of the diaphragm from conditions like ascites, severe bowel dilation and at times painful abominal conditions results in lower inspiration volumes and faster breathing rates and ensuing fatigue from that
#4. 62/F admitted for CHF exacerbation with Dyspnea needing 4L O2 via Nasal Cannula. Improving with IV Lasix BID diuresis. By Day 3, feels short of breath, weak. But is now off Oxygen now , Lungs + Heart sounds clear, Edema mild, Labs: WBC 7K, HgB 13, Na 130, K 1.9, CO2 28, Creatiine 1.1, BUN 25, LFTs normal. CXR clear !
Diaphragm muscle is sensitive to potassium, low phosphorous and severe malnutrition states and this weakness manifests in increased work of breathing.
Diuresis caused loss of potassium in her, one reason to monitor electroytes during aggressive diuresis
Don’t miss these fun posts! Subscribe via email 📩 | |




